Admin |
October 18, 2021
October is International Stuttering Awareness Day. In light of this, we teamed up with Janet Stevens to bring you an informative article on Stuttering. Janet is an experienced speech and language therapist, independent practitioner and module leader on our Speech, Language and Communication Needs module.
This article highlights the different terminology you may hear, important facts, risk factors, and much more. If you are interested in any of the information below, please do feel free to leave any questions or feedback for Janet in the comment section at the end of this article.
Raising awareness on International Stuttering Awareness Day
Firstly, it is important to understand the differences in terminology: the speech difficulty known as stuttering in the USA & Australia, is more commonly referred to as stammering in the UK. The charity that supports & provides guidance for families, education & health agencies that have contact with children & adults who stammer in the UK is known as STAMMA. All of these terms can equally be encompassed within the descriptor of dysfluency.
Stammering is a neurophysiological speech disorder that appears to affect neural pathways in the speech-linked areas of the brain; it can be described as being like ‘a glitch in the wiring’.
A current definition of stammering is:
A voluntary disruption to the smooth flow & timing of speech, characterised by prolongation or repetition of sounds, blocking or secondary features.
This is what we know about stammering:
- It affects 5% of children under 5 years of age
- It affects 1% of the adult population
- It usually first manifests between the ages of 2 and 5 years of age
- It is not linked in any way to intelligence (IQ)
- It can be intermittent & appear to disappear for periods of time
- Early identification & referral to a Speech-Language Therapist (SLT) is essential to monitor & assess risk factors
Main Risk factors
- Family history of stammering: hereditary factors particularly strong with male relatives, although females can stammer
- Recognised difficulties with early speech/language/communication development OR significantly advanced language skills
- Time since onset of stammer: the longer the period of time between onset & consultation with SLT, the greater the risk that the stammer will become established
- Pattern of change over time: if child stammers every day, the risk of more permanent stammering is increased
- Parental levels of concern: the more anxious & concerned parents are, the greater the potential risk that early mitigating factors will not be effective
- Child awareness/level of concern: the higher child levels of concern/anxiety, the greater the risk that the stammer will become established
Triggers for Stammering
Multiple factors can interact with these main risks to trigger a stammer at any time; the circumstances will vary for individual children; however, none of these factors will cause stammering by themselves; individual children will already have an underlying deficit or predisposition or a stammer.
The factors to consider are:
- Language factors
- Psychological factors
- Environmental factors
- Physical factors
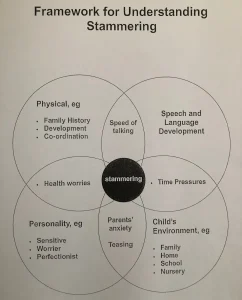
There is a Framework for Stammering that is used by the majority of NHS SLT teams & alternative diagnostic agencies, to inform their thinking about the specific factors involved in the stammer of individual children
This is also known as the Multifactorial Model: as the graphic illustrates all 4 factors interlink & overlap. SLTs will use this information to generate a Profile of Risk for each child, which will then inform the focus of intervention & act as the evaluation framework for that intervention.
Features of Stammering
- Repetition of sounds [usually word initial]: e.g. m.m.m.mummy
- Prolongation of sounds [usually word initial]: e.g. sssssunshine
- Blocking of sounds: e.g. trying to speak but no sound comes out
- Secondary features: e.g. eye blinking, twitching, facial grimaces
This list is a broadly chronological pathway of the typical evolution of childhood stammering. In terms of identification, generally stage 1 is auto-resolvable, whereas once stages 2/3 are reached, the risks multiply & the likelihood of the stammer becoming established is significantly increased.
Prevalence
Of the 5% of affected children:
- 2 of the 5 will experience transient difficulties with dysfluency between the ages of 3-5, which will resolve with no external intervention
- 2 of the 5 will experience significant dysfluency as young children, which will be resolvable via SLT intervention & guidance
- 1 of the 5 will become a chronic stammerer, through childhood into adulthood
Intervention Options
- Indirect Intervention: this could include guidance/advice for the family & ‘watchful waiting’ by the SLT, who would over review appointments if the family requested them
- Direct Intervention: the care pathways on offer across different NHS trusts in the UK will vary. In my own Trust, SLTs are trained to offer Parent Child Interaction sessions, Lidcombe Therapy sessions, Swindon Group Therapy sessions and referral to specialist intervention at The Michael Palin Centre in London. An individual child (& their family) will be guided onto one of these options initially, with the possibility of moving onto other options at a later date. This is not a sequential pathway, as each individual child & family are unique, so therapy packages will be uniquely designed around their needs.
Parent-Child Interaction
This intervention is based within the Hanen Approach: essentially it comprises short video clips of interactions involving a parent/significant adult & the child, which are then watched by the adult with discussions guided by the SLT to help identify areas of interaction ‘practice’, which could be ameliorated or changed, by the adult to minimise the child’s stammering behaviour [referring to the Profile of Risk].
Lidcombe Programme
This is a behavioural treatment mainly for children under 6 who stammer; there is no pressure within the treatment sessions on the child to consciously attempt to change any stammering behaviours. Parents are ‘trained’ to identify the number/severity of every stammered utterance [called ‘offering verbal contingencies’]; they do this in daily ‘treatment’ sessions AND in some ‘natural’ conversations. [https://www.lidcombeprogram.org]
Swindon Group Programmes
The SLT team in Swindon have devised, operated & trained other SLTs in a series of 3 different group therapy programmes. They combine intensive speech therapy in a group of peers with similar impairments with outdoor activities. These can be used sequentially & generally cover the ages from 6 up:
- The Smoothies Pack (6-9 years)
- The Blockbuster Pack (9-12 years)
- The Teens Challenge Pack (13-17 years)
[https://thefluencytrust.org.uk]
The Michael Palin Centre
As a centre of excellence in London, the team of highly skilled SLTs deliver intensive 2-week programmes for the families of the stammering child, as well as the child themselves. Group discussion, parent support and techniques to reduce stammering behaviour, combine in a challenging yet supportive environment to resolve often deep-seated family & personal issues, of which the stammer is frequently a manifestation. These courses require referral & local GP/NHS funding, so it can require years of effort to secure a place.
Advice for Parents and Supporting Adults (e.g. teachers)
- Remain open to communication about the STAMMER
- Do not react to the STAMMER in a negative way
- Wait for the child to finish talking, don’t interrupt or finish their sentences for them
- Don’t ask the child to stop & start talking again
- Praise the child for things they are good at/do well, using specific praise
- Praise the child when they talk ‘fluently’ or ‘smoothly’
- Maintain eye contact when communicating with the child whenever they stammer
- Slow down your own rate of speech
- Use pauses to give the child time to think & process information
- Don’t ask too many questions; use comments instead
In conclusion, if, as a professional educator, parent or relative, you become aware of a child stammering, please refer or encourage parents to refer the child immediately. The closer to onset a child can be seen by an SLT, the better the long-term outcome will be.





What do you think?